While COVID-19 respiratory features such as cough, pyrexia, and dyspnea are well-known, emerging research has shown that the virus can also affect the gastrointestinal (GI) tract. A meta-analysis of many recent studies estimates that 17.6% of COVID-19 patients have gastrointestinal manifestations. COVID GI symptoms can range from mild diarrhea to severe complications such as intestinal bleeding and perforation.
Here we explore the latest research on COVID stomach issues, including how it affects the gut, associated intestinal issues, and how clinical laboratories can diagnose COVID gastrointestinal infections.
How Does COVID Affect the Gut?
COVID-19 impacts the gastrointestinal tract and its microbiome in the following ways:
- It changes the intestinal lining: According to a study supported by several NIH institutes, COVID-19 harms the gut microbiome by altering the gut lining in a way that allows dangerous bacterial pathogens to enter the bloodstream and cause additional infections.
- It materializes with bothersome clinical manifestations: Another study published in the American Journal of Physiology suggests COVID-19 can cause gastrointestinal manifestations such as nausea, emesis, and diarrhea.
- It compromises the intestinal barrier: The same American Journal of Physiology study also found that the virus can infect the cells that line the intestines, leading to inflammation and damage to the intestinal barrier.
- It can persist and lead to clinical manifestations that impact patients’ quality of life: A report from Harvard Health highlights emerging evidence suggesting that GI problems may persist in some patients who have had COVID-19. The report proposes that persistent COVID can affect the gut and cause clinical manifestations such as abdominal pain, diarrhea, and changes in bowel habits.
- It disturbs the gastrointestinal microbiome: A study from the National Institute of Health indicates that COVID-19 disturbs the gut microbiome, allowing bacterial pathogens to flourish. The report suggests that the virus can also disrupt the intestinal lining, potentially allowing these bacterial pathogens to become bloodborne and lead to risky secondary infections.
What Are the Intestinal Issues Associated With COVID?
Those with serious COVID-19 are at an even higher risk of developing gastrointestinal problems. During their often lengthy hospitalization, 74-86% of critically ill patients with COVID-19 present gastrointestinal issues affecting the liver, gallbladder, pancreas, and intestines.
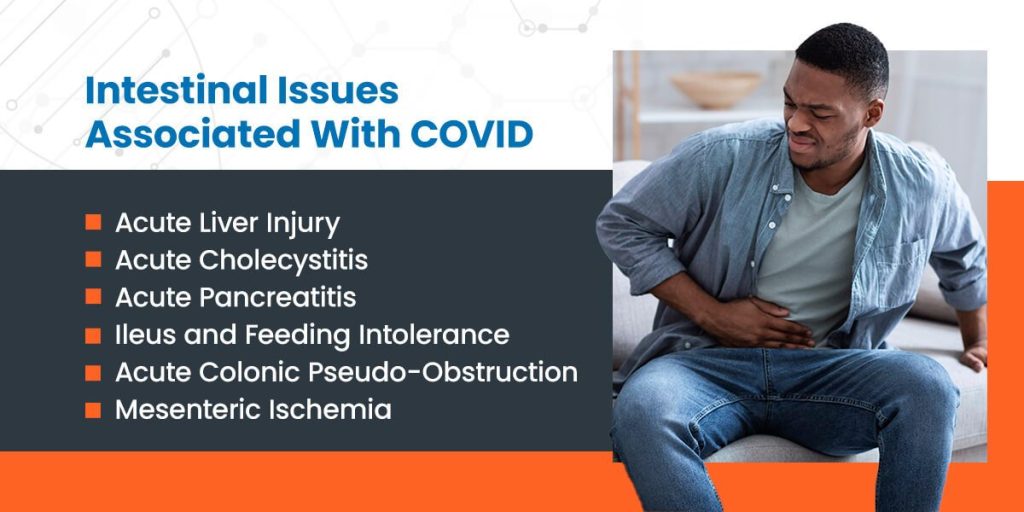
Acute Liver Injury
According to research, around 66% of patients with severe COVID-19 experience increased liver transaminases, with the average levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) exceeding 400 units per liter of serum. In rare cases, the liver injury may even lead to liver ischemia.
Although the exact cause of acute liver injury in COVID-19 patients is unclear, researchers believe multiple factors are at play. Some studies have indicated that the extent of transaminase elevation may be a predictor of disease severity and an independent predictor of mortality.
Acute Cholecystitis
COVID-19 patients, particularly those critically ill, have frequently been diagnosed with acute cholecystitis. In most cases, the cholecystitis is acalculous, and its exact cause is not fully understood. Although decreased gallbladder wall movement is common in critical illness, a viral role in the pathophysiology of cholecystitis in COVID-19 patients has not been ruled out.
Acute Pancreatitis
Acute pancreatitis is another common diagnosis in patients critically ill with COVID-19. In some cases, the pancreatitis has progressed to necrotizing pancreatitis, which requires percutaneous, endoscopic, or surgical debridement. While COVID-19 may directly cause acute pancreatitis in these instances, the link between the virus and acute pancreatitis is not yet fully understood.
Ileus and Feeding Intolerance
Approximately 50% of critically ill COVID-19 patients admitted to the ICU experience ileus and feeding intolerance — anorexia is the most common GI manifestation of active COVID-19. The cause of the ileus is likely due to multiple factors, as these patients often require high doses of sedatives and opioids to synchronize with ventilators, which can slow intestinal function. Nevertheless, a specific cause related to COVID-19 may also contribute to the ileus, although this has not been definitively established.
Acute Colonic Pseudo-Obstruction
Several studies have reported a unique colonic syndrome in critically ill COVID-19 patients. This syndrome is characterized by severe gaseous distention without apparent distal obstruction, similar to acute colonic pseudo-obstruction or Ogilvie’s syndrome. It is unclear whether this syndrome is specific to COVID-19 or a manifestation of protracted critical illness.
Mesenteric Ischemia
Mesenteric ischemia is the most severe gastrointestinal complication observed in critically ill COVID-19 patients. In cohort studies of COVID-19 patients admitted to a single institution, mesenteric ischemia was reported to be 3.8-4%. However, early diagnosis based on physical examination and classic symptomatology is not often feasible since most of these patients are sedated, require mechanical ventilation, and are on low-dose vasopressors, precluding reliable clinical evaluation.
Instead, the most common presenting signs are new feeding intolerance, abdominal distention, increasing leukocytosis, increasing vasopressin requirements, and unexplained metabolic acidosis.
How to Diagnose COVID-Related GI Issues
Diagnosing gastrointestinal complications in COVID-19 patients promptly is critical to prevent further morbidity and mortality. However, diagnosing COVID-related gastrointestinal issues can be challenging as the clinical manifestations are non-specific and can be attributed to various other conditions.
Still, healthcare professionals should maintain a high index of suspicion for GI complications in COVID-19 patients presenting with new-onset gastrointestinal concerns or worsening of preexisting symptoms. In addition, medical professionals should consider the patient’s clinical presentation, laboratory findings, and imaging studies to establish a diagnosis.
Laboratory Studies
Laboratory studies, including complete blood count (CBC), comprehensive metabolic panel (CMP), and coagulation studies, can help identify patients at risk of developing GI complications. Elevated lactate levels may indicate mesenteric ischemia, while increased inflammatory markers such as C-reactive protein and procalcitonin may suggest infectious colitis.
Imaging Studies
Imaging studies such as abdominal X-rays, CT scans, and ultrasounds can help diagnose GI complications. Abdominal X-rays can detect bowel distention and air-fluid levels, while CT scans can reveal bowel wall thickening, pneumatosis, and portal venous air. Ultrasound can detect bowel dilation, wall thickening, and mesenteric ischemia.
Endoscopic Evaluation
Endoscopic evaluation, including upper endoscopy and colonoscopy, can provide direct visualization of the GI tract and identify mucosal abnormalities such as ulcers, erosions, and bleeding. However, endoscopy should be reserved for patients with severe GI symptoms or suspected GI bleeding.

Detect COVID-Related GI Complications With Applied BioCode’s Gastrointestinal Pathogen Panel
Our gastrointestinal pathogen panel is a molecular test that detects and identifies the most common causative pathogens in raw stool or stool in Cary-Blair medium from symptomatic patients. The panel is a flexible, cost-effective, and comprehensive assay that uses multiplex technology to detect up to 17 different pathogens simultaneously.
The FDA-cleared GI pathogen panel works by detecting the RNA or DNA of pathogens, including viruses, bacteria, and parasites, in a single sample. Our GI pathogen panel is key for healthcare professionals wanting to provide a faster and more accurate diagnosis to enable appropriate treatment. Contact the Applied BioCode team today to learn more about our products and technologies.


