Table of Contents
- Strategic Planning and Budgeting
- Compliance and Regulatory Considerations
- Instrumentation and Equipment Needs
- Supply Chain Management
- Standard Operating Procedures (SOPs)
- Data Management and Digital Solutions
- Quality Assurance, Control, and Evaluation
- Documentation and Reporting Protocols
- Staff Training and Competency Development
- Continuous Monitoring and Assessment
Implementing a new diagnostic test in your laboratory can be transformative. It allows you to improve patient care and expand your services and offerings. Although documented proof is a requirement for regulatory bodies, the ultimate goal of validation is to ensure reliable results for patient outcomes. As such, test method validation will require careful planning and ongoing quality assurance to meet compliance and ensure reliable diagnostic outcomes.
Strategic Planning and Budgeting
Diagnostic assay validation encompasses more than the technical aspects. It also requires assessing quality metrics like desired turnaround time, obtaining positive samples, a result reporting framework, customer service, and budgeting.
Consider expenses like reagents, equipment, personnel training, and regulatory fees associated with test method validation. If you are implementing a high multiplex panel, you might need to apply for the DEX Z-Code®, depending on your region. Refer to your regional reimbursement guidelines to make sure, as this can impact your budgeting. DEX Z-Code® provides a standardized way to bill these high multiplex panels to help with reimbursement.
If you plan to adopt a molecular diagnostic test for infectious diseases, read up on the MolDX reimbursement criteria to learn more about the process. The program will show you the documents and requirements needed to qualify your test for insurance, meet compliance, and justify claims.
Learn More About MolDX Reimbursement
Compliance and Regulatory Considerations
When implementing a new laboratory test, you need to follow assay validation guidelines set by regulatory bodies. Key regulations dictate how to validate a new lab test effectively, which can protect your patient’s safety and your lab’s credibility. The compliance process generally includes the following:
- Consultations with regulatory authorities: Consult with regulatory authorities to learn about importation requirements. Collaborate with manufacturers to ensure that you understand your registration requirements.
- Validation studies: For commercial tests, it is essential to evaluate the assay’s sensitivity, specificity, and overall accuracy both in local settings and large-scale clinical contexts. This also includes large-scale assessments for tests outside their intended scope and smaller studies for commercial tests.
- Work closely with regulatory authorities: After evaluating your test’s performance, you will need to work closely with regulatory authorities and manufacturers. Consider the extra time it may take to submit your application and meet supplementary evidence provisions.
Instrumentation and Equipment Needs
You will need the right technology to validate a new assay, including analytical instruments, quality control tools, and data management software. Your equipment should:
- Be compatible with existing systems.
- Be easy to use and train personnel on.
- Come with manufacturer support.
Investing in high-quality instrumentation can make the validation process easier while enhancing assay performance.
Supply Chain Management
Establish relationships with reliable suppliers when implementing a new lab test. This will make supply chain management much easier, as you will know you have the right reagents and materials when needed.
Develop robust logistic strategies to ensure consistency in the supply chain. Regularly assess supplier performance to prevent disruptions and ensure reliability when validating your test. A reliable supplier ensures consistent access to high-quality tools.
Effective storage is also crucial, as you will need somewhere to store positive samples and other reagents during validation. Request a detailed checklist from the manufacturing company that covers the necessary space, ventilation, power, and other technicalities you need.
Standard Operating Procedures (SOPs)
Standard operating procedures (SOPs) are the steps of your validation process. Following them helps ensure consistency and reliability. When documenting your methods, record results meticulously during the validation process to maintain transparency and accountability. This practice will help you meet compliance while being a good reference for future validations.
Data Management and Digital Solutions
Data management is a crucial aspect of assay validation. It includes tracking performance and results during the validation process. The essential step can help you keep diagnostic integrity, meet compliance, and ensure quality control measures. Some digital tools can streamline the process and help you monitor assay performance over time.
Quality Assurance, Control, and Evaluation
Ongoing quality control practices ensure that your validated tests remain reliable and accurate over time. A comprehensive quality assurance program might include:
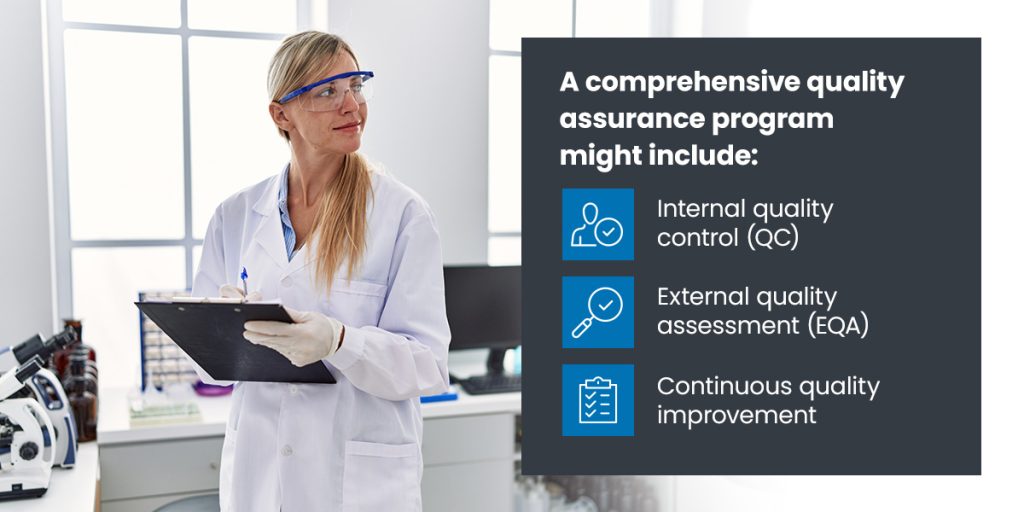
- Internal quality control (QC): This includes monitoring your analysis processes to detect errors before reporting results.
- External quality assessment (EQA): EQA involves testing proficiency and lab comparisons to identify deficiencies.
- Continuous quality improvement: On-site supervisory visits can include routine monitoring of quality indicators. This helps review performance over time and take corrective actions to improve.
Documentation and Reporting Protocols
Recording and reporting your validation processes is crucial for meeting regulatory requirements. Proper documentation provides evidence of compliance during audits or inspections. Effective documentation includes keeping clear records of all findings related to the validation process, such as:
- Raw data
- Analysis results
- Deviations from protocols
- Any corrective actions taken
Additionally, if your lab is registered under the College of American Pathologists (CAP), you must mention the new test and provide a proficiency survey to show that it meets standards and is validated properly.
Staff Training and Competency Development
Successful implementation of a diagnostic test relies on the training and expertise of your lab personnel. This is especially true for high-complexity testing. Keep your staff well-versed in protocols to enhance the reliability of your validated assay. Ensure personnel undergo thorough training on assay protocols and quality assurance activities.
Conduct routine competency assessments and proficiency testing. That way, you can make sure your staff has the right skills for consistent, high-quality test performance. You might also establish an ongoing education program to keep everyone updated on best practices.
Continuous Monitoring and Assessment
Establish key indicators and milestones during the planning phase to implement your test successfully. This is especially true in tests related to drug resistance detection, such as infectious diseases where drug resistance poses significant public health concerns.
When a lab introduces a new test, especially one relevant to drug resistance detection, it is responsible for informing the state public health lab. Most states maintain lists of reportable diseases and tests, which include requirements for monitoring drug resistance, particularly for diseases where laboratories must report findings of resistant strains to state health authorities for public health tracking.
Include a robust framework for evaluating the test’s impact, or the following indicators:
- Purpose
- Targets
- Data elements
- Sources
- Calculation methods
Creating feedback loops will also help you refine your procedures. Regularly engage with staff about their experiences, and you’ll gain valuable insights into areas needing improvement. Analyzing your indicators can clarify the test’s impact on patient outcomes. It can also reveal areas to improve and enhance effectiveness.
Implementing a maintenance plan is important for bringing on a new test. Applied BioCode Inc. provides dedicated service engineers to assist with technical and other support issues.
Why Trust Us?
Applied BioCode Inc. has extensive expertise in diagnostic testing solutions, including tailored solutions for laboratories looking to validate new assays. We specialize in high-throughout syndromic panel testing for infectious diseases. Our commitment to advancing molecular diagnostics is evident in our flagship products, the BioCode® Respiratory Pathogen Panel (RPP) and the BioCode® Gastrointestinal Pathogen Panel.
Our product harnesses Barcoded Magnetic Bead (BMB) technology, integrating digital barcodes with molecular and immunochemistry for accuracy and efficiency. With high throughput, flexible reporting options, and parallel testing capabilities, our platform ensures rapid and reliable results for medical providers. We are also happy to guide support for validation and customer support documents.
Our dedication to quality assurance, innovative technologies, and comprehensive support positions us as a trusted partner in your diagnostic test development journey.
Jump-Start Your Validation Testing With Applied BioCode Inc.
Adopting a new diagnostic test can enhance patient care and expand your laboratory services, but it requires careful planning and meeting regulatory standards. With Applied BioCode Inc., you gain access to advanced diagnostic solutions like the BioCode® Respiratory Pathogen Panel, which efficiently detects 17 viral and bacterial pathogens from a single sample, ensuring rapid and reliable results.
Ready to transform your laboratory’s capabilities? Contact us today to learn how our innovative technologies and comprehensive support can help you successfully validate and implement new assays in your lab.